A guide for implementing telehealth and exploring your options.
In most settings, physical, occupational, and speech therapy require close proximity between a patient and provider. The therapist may need to manually stretch muscles, observe swallowing, or help the patient balance as they exercise. However, limiting patient encounters to in-clinic only can inadvertently hold your clinic back from helping more patients.
While remote and virtual rehab therapy is nothing new to the industry, it was a very new experience for many outpatient rehab therapists when the COVID-19 pandemic shut down the world. Suddenly, patients and providers couldn’t be in the same room together, but the therapy and healing needed to continue. With quick pivots from CMS and other insurance providers, telehealth rehab therapy became the norm for a short time.
As the world returns to a more in-person pace, outpatient rehab therapists can choose to add telehealth as an adjunct to their practice. For many patients, including those with chronic illnesses, telehealth can be a more convenient and economical option compared to traditional in-person care. In this guide, we walk you through the various types of telehealth that are available through the public health emergency (PHE) and highlight how one clinic was able to pivot during the pandemic and create a brand-new telehealth program from scratch.
Types of telehealth
Because of the COVID-19 crisis, CMS expanded their coverage of some virtual visits, or “e-visits” to physical therapists, occupational therapists, and speech-language pathologists, effective immediately. Special HCPCS codes have been published for e-visits and details about the requirements and reimbursement are included below. According to a fact sheet released by CMS, e-visits are “non-face-to-face patient-initiated communications through an online patient portal.”
Telehealth visits
Telehealth services require “interactive audio and video telecommunications system that permits real-time communication between the distant site and the patient at home” and providers may “include physicians, nurse practitioners, physician assistants, nurse midwives, certified nurse anesthetists, clinical psychologists, clinical social workers, registered dietitians, and nutrition professionals.”
- Mode of communication: Real-time, synchronous teleconference.
- Type of service: A visit with a new or established patient using telecommunication systems.
- PT/OT codes: 97110, 97112, 97116, 97150, 97530, 97535, 97542, 97750, 97755, 97760, 97761
- SLP Codes: 92507, 92508, 97521, 97522, 97523, 97524
Virtual check-ins
Virtual check-ins are defined as a “brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image.”
- Description: Brief communication technology-based service, e.g. virtual check-in, by a physician or other qualified health care professional who can report evaluation and management services, provided to an established patient, not originating from a related evaluation and management service provided within the previous 7 days nor leading to an evaluation and management service or procedure within the next 24 hours or soonest available appointment.
- Mode of communication: Audio only via telephone or exchange of information through video or image.
- Type of service: Brief communication initiated by the patient to help determine whether they need to be seen for a full evaluation or treatment service.
- Code: G2012
Remote evaluation of patient videos and/or images
CMS allows clinicians to bill for remote review of prerecorded images and videos from the patient.
- Description: Remote evaluation of recorded video and/or images submitted by an established patient (e.g., store and forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment.
- Mode : Asynchronous portal.
- Type of service: Interpretation of video/image.
- Medicare code: G2010
Telehealth assessments
Telephone assessments can be used for lengthier discussions to address more complex or emergent issues identified by the patient or caregiver or when the patient does not have access to other modes of communication technology, such as a patient portal.
An important note: Telephone assessments may also be used for self-care/home management training (e.g., activities of daily living (ADL) and compensatory training, meal preparation, safety procedures, and instructions in use of assistive technology devices/adaptive equipment) direct one-on-one contact, each 15 minutes. Code: 97535
- Description: Telephone assessment and management service provided by a qualified nonphysician health care professional to an established patient, parent, or guardian not originating from a related assessment and management service provided within the previous 7 days nor leading to an assessment and management service or procedure within the next 24 hours or soonest available appointment.
- Mode of communication: Audio only via telephone or telecommunication device.
- Type of service: Telephone assessment and management.
- Codes: 98966, 98967, 98968
E-visits
Qualified non-physician online assessment (Medicare) or qualified non-physician online evaluation and management (non-Medicare), for an established patient.
- Description: E-visits describe brief, online assessments that are reported for cumulative time spent over the course of up to 7 days.
- Mode of communication: Asynchronous portal.
- Type of service: Brief, online assessment.
- Medicare codes: G2061, G2062, G2063
- Equivalent non-Medicare codes: 98970, 98971, 98972
E-visits may only be used for established patients, meaning that the patient already has a plan of care and is known to your practice.
Providers may tell a patient that e-visit services are available, but the patient must request the service. There are three e-visit codes. Each code may be billed based on the cumulative time of the e-visits over 7 days. The most practical way to utilize these new codes is to limit “e-visits” to once weekly.
- G2061: 5-10 Minutes of cumulative time in a 7-day period
- G2062: 11-20 minutes of cumulative time in a 7-day period
- G2063: Over 20 minutes of cumulative time in a 7-day period
Clinicient will be setting up specialized clinical content and charge capture rules to support these requirements. When this setup is completed, a therapist may document the e-visit normally, then indicate the appropriate e-visit code based on the cumulative time. Your EMR and billing system should automatically roll the time spent providing services into the selected e-visit code.
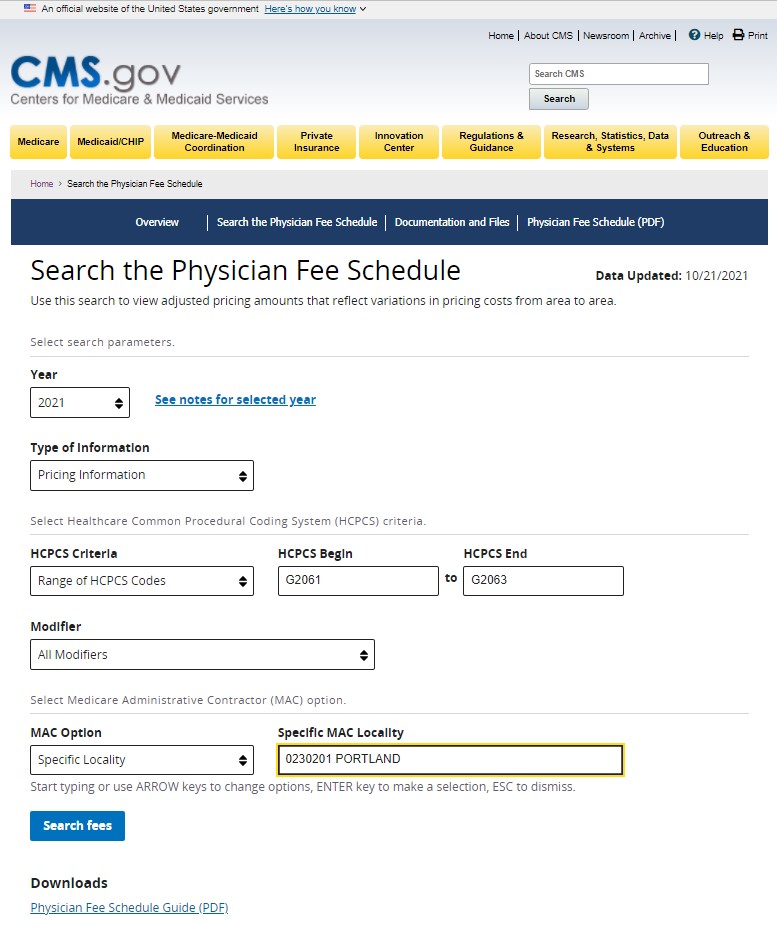
Finding the right HCPCS codes
The HCPCS codes for e-visits are included in the Medicare Physician Fee Schedule. Here is an example of using the Physician Fee Schedule Search tool. (Search for Pricing information for a range of HCPCS codes for your specific locality.)
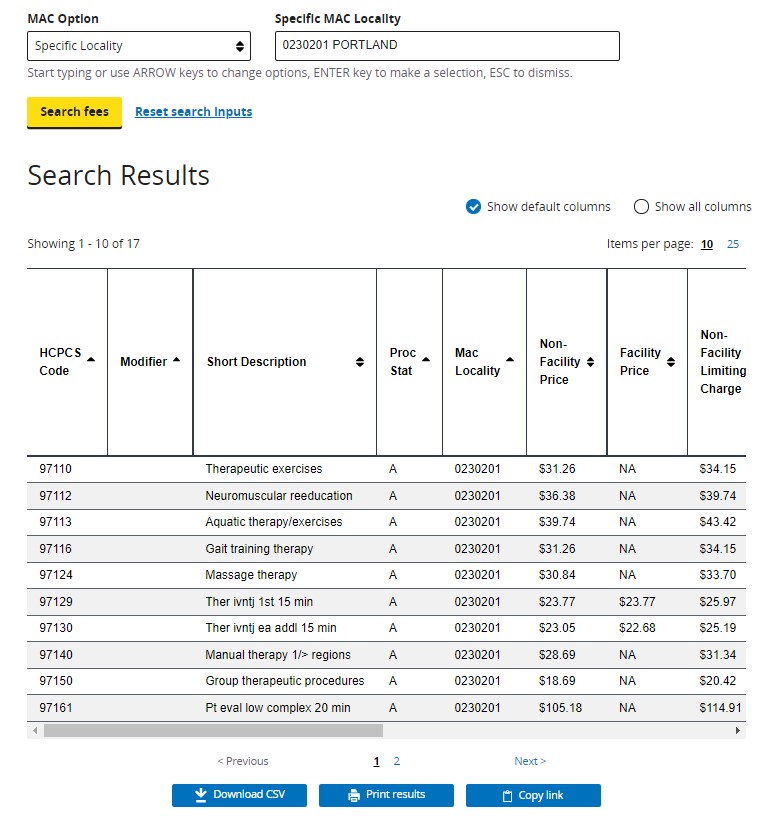
Here is an example search for the e-visit codes for Portland, OR:
Documenting telehealth and e-visits in Insight
The Insight Platform supports scheduling and hosting a telehealth session, and provides e-visit charge capture for billers. For therapists, you simply need to document the services provided remotely along with the appropriate e-visit code to indicate the cumulative minutes spent providing the service over a 7-day period. The platform will automatically roll the minutes spent providing traditional services into the selected e-visit code.
In this example, the therapist provided exercise instruction, neuromuscular re-education, therapeutic activities, and some ADL training during the virtual visit.
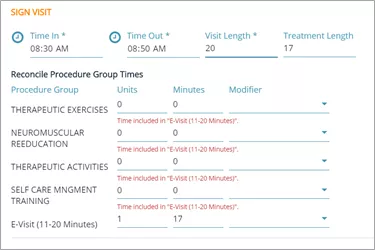
The therapist documented those services as they would normally but added the e-visit procedure indicating that between 11 and 20 cumulative minutes were spent providing services.
The system automatically rolled the standard CPT codes into the e-visit HCPCS code.
For more information on the types of allowable e-visits and applicable codes, please see the CMS Telehealth Fact Sheet.
Implementing telehealth: a Connecticut case study
Telehealth is not a new concept to the healthcare industry. In fact, some medical providers have been administering telehealth visits for years.
But when the COVID-19 pandemic arose and states began mandating social distancing rules, Sport & Orthopaedic Physical Therapy in Connecticut found themselves needing a new way to treat patients – and fast. Without the ability to hold in-clinic visits full-time, therapist and practice owner, Paddy Jarit, was faced with the task to find alternative treatment options to support their patients and guide them to a full recovery.
Launching the program
In response to the pandemic, Jarit closed his clinics, researched his options, and launched his physical therapy telehealth program in just four days.
To be effective in providing virtual care physical therapy, the most important part of launching a successful telehealth program is the relentless focus on the relationship between patient and provider. Jarit comments, “Even though the interaction is virtual, the relationship must be personal.” Using telehealth technology, the Insight Platform, and a clinical process followed by his entire staff, Jarit was able to successfully initiate a telehealth program.
The implementation process
(Pssst… We provide a more in-depth implementation process, plus thoughts on the benefits and future of telehealth for outpatient rehab therapy, in our free telehealth download.)
- Review rules, regulations, and payer coverage
-
- Know the laws in your state related to telehealth coverage and compliance.
- Tip: Research common payers, including Medicare and commercial payers, to ensure telehealth is covered and claims are less likely to be denied.
- Research your patient market
-
- Consider potential barriers or limitations that may impact patients, like internet access or functional limitations.
- Tip: Patients with busy schedules, kids, or long commutes may be more likely to attend telehealth visits.
- Research and choose your telehealth provider
-
- Consider if the software is user-friendly for both staff and patients.
- Tip: Some telehealth providers offer additional perks that may benefit your clinic, like additional security features or online scheduling options.
- Train your staff
-
- Encourage dialogue between providers and ask staff to share tips so everyone becomes more familiar with the software.
- Tip: Allow team members to test the software at least once before their first patient visit.
The patient process
- Schedule the patient
-
- Schedule each patient for 45 minutes with a five-minute window in between appointments.
- Tip: Use two monitors during the online physical therapy visit – one for documentation, the other for patient interaction.
- Provide patients with step-by-step instructions
-
- Instructions should communicate to the patient where they need to go (URL), when they should arrive (ex: 5 mins before), and how to set up audio and video connections on their phone or preferred device.
- Tip: Include directions on how to test audio and video settings prior to the session.
- Require a right-to-treat consent form before the appointment starts
-
- Require patients to sign and return a consent form before the appointment so the therapist can get right to treatment without having to wait on paperwork.
- Tip: If the patient doesn’t have a scanner, a cell phone photo of the consent form works just as well.
- Use a virtual waiting room
-
- Use a virtual waiting room so staff can acknowledge the patient has arrived just like they would in the front office.
- Tip: Most teleconferencing platforms offer a waiting room feature.
- Follow up with a telehealth playlist
-
- Be sure to send the patient any exercise videos or extra curricular resources so they can keep building strength at home. To make it super easy for your patients to find the videos, put the exercises up on your company YouTube or Facebook account.
- Tip: Use the videos to coach patients on how to complete their exercises from the safety of their own home.
Inspiring results and engaging patients in their home
Overall, in their short experience with telehealth, Jarit and the entire team at Sport & Orthopaedic Physical Therapy are each effectively treating patients virtually and have experienced a high level of receptiveness and appreciation from their patients.
Jarit notes, “Patients have more than welcomed me into their homes through telehealth physical therapy. The most common comment has been that they’re thankful that I can watch them do their exercises at home while fine-tuning their technique.“
With the help of telehealth, Sport & Orthopaedic Physical Therapy successfully arrived 217 patients in the month of April 2020, which is nearly in line with their pre-pandemic, January 2020 numbers of 235 patients.
To his credit, Jarit has taken time to share his telehealth experiences with the rest of the outpatient rehabilitation community. As an active participant in Clinicient’s COVID-19 Town Halls, Jarit has been a consistent and generous contributor to the telehealth conversations. Although crisis invites change, as an industry, we’re learning as we go and sticking together in the process.
The future of telehealth in outpatient rehab therapy
Telehealth may be a relatively new concept to the physical therapy space, but it doesn’t appear to be going anywhere even after COVID-19. Post outbreak, 90% of hospitals expect greater use of telehealth to persist. Clinics like Sport & Orthopaedic Physical Therapy have embraced telehealth in a very short time and will only become more skilled at delivering effective virtual care over time.
Jarit adds, “if the insurance industry realizes the value of telehealth PT I undoubtedly see this as an adjunct to my in-clinic physical therapy.” Patients don’t have to lose their momentum towards a full recovery just because there’s a pandemic, and providers can continue to be effective in their care without face-to-face interaction. Telehealth is here to stay and will continue to transform the outpatient rehabilitation industry.



Comments