A key component of transitioning into a value-based care model is knowing how to collect and manage patient data. And in our increasingly data-driven world, understanding the nuts and bolts of data is important. But with so much data out there, where can clinics get started?
The subject of our most recent Industry Town Hall focused on collecting and managing outcomes, with special guest Stephen Hunter (DPT, OCS, FAPTA), the Rehab Services Director with Intermountain Healthcare. Along with our host Jerry Henderson, PT, the two discussed how outpatient rehabilitation therapists are primed for illustrating the value of their care with patient outcomes data. Since 1999, Intermountain Hospital has been perfecting its patient outcomes collections process, and Stephen Hunter offered some great advice to help clinics start the process.
Why should you collect patient outcomes?
Collecting outcomes is an essential component of value-based care. However, there are plenty of other reasons why clinics should collect patient outcomes. Here are six that Dr. Hunter shared at the Town Hall.
- Outcomes can improve patient care: Collecting outcomes data provides clinics with the information they need to visualize and analyze the effectiveness of their care. With more data, therapists can learn what’s ineffective, what needs updating, and the best course of action for patient care plans.
- Data can determine strategic priorities for your clinic: Data collection is great for noticing patterns. Dr. Hunter offered an example from his clinic, where declining outcomes data showed they weren’t providing the needed information when handing off patients to home-care or other outpatient teams. By noticing that trend, they could focus on the whole patient journey and close any provider communication or documentation gaps.
- Data also determines professional development priorities: Similarly, therapists can use data to educate, share successes, and share failures with fellow therapists for professional development. Dr. Hunter’s team often hosts 90-minute presentations with therapists to share tips on clinic skills, outcome trends, and performance.
- Outcomes can improve patient engagement: While patients may verbally say they’re “feeling good,” outcomes data can provide more clarity. Therapists can then use the data they notice—like less pain but more functional limitations, for example—to investigate the cause and adjust their patient’s care plan as needed. The patient can feel more engaged when they trust the expertise of their therapist.
- Provider communication can improve when outcomes are tracked and shared: When providers need to hand-off patients to another provider, offering that patient’s outcomes data will illustrate a complete picture of their care plan. Providers can also use outcomes as evidence for effective therapy methods or care plans when communicating with their peers.
- Data and outcomes can showcase your clinic’s value: Outcomes are a potent method for demonstrating the value of a clinic and its services.
How can you successfully measure outcomes?
Every clinic is different, which means success will look different, too. Luckily, groups like Intermountain Hospital have been collecting outcomes for over 20 years and have learned a lot along the way. Dr. Hunter shared his advice for how Intermountain has succeeded in measuring outcomes.
- Classify groups and focus on the patients: The priority should always be on the patient and meeting their needs. Additionally, Intermountain typically groups patients so they can compare outcomes and progress when analyzing their care plans. Dr. Hunter recommended avoiding grouping by ICD-9 or ICD-10 codes, as that can get complicated. Instead, group patients by what makes sense for the clinic, whether that’s patient injury type, age, care plan, etc.
- Choose outcomes to measure: When first starting, Dr. Hunter recommends choosing at least one outcome to track and reporting the patient’s status at every visit. Common outcomes examples include:
- Pain level based on area and position
- Mobility or functionality level based on area and position
- Reflex responsiveness
- Interference with work, leisure, or regular activities
- Time it takes to stand, walk, or perform an activity
- Define the clinic’s outcomes purpose: Therapists should consider why they’re tracking outcomes, how they want to track them (whether digitally or manually), and how it will impact their services. Dr. Hunter recommends focusing on condition-specific outcomes that are generic and performance-based.
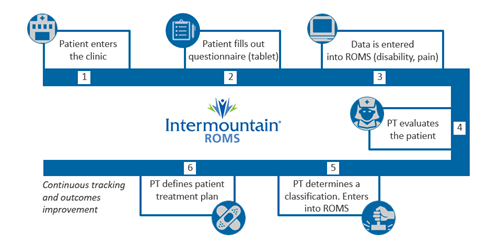
- Create a clinic process: Creating a process will ensure outcomes are collected correctly and on time. Additionally, all members of the clinic should be committed to the process. At Intermountain Healthcare, their approach works as follows:
- Patient enters the clinic and is asked to complete a questionnaire on a tablet.
- Responses are automatically recorded in their system once the patient submits them.
- Provider reviews responses and meets the patient. They can discuss any issues during the appointment.
- The provider determines an injury classification, defines the care plan, and enters information into their database.
- The clinic continuously tracks patient outcomes with every visit and adjusts the care plan as needed.
- Keep it simple: Dr. Hunter warned against getting too complicated with outcomes. By keeping the outcomes collection process relatively simple, therapists won’t feel too burdened with extra administrative steps that could take away time from their patients. Plus, with outcomes collection and measurement solutions like Keet Health, most of the process can be automated for further simplification.
- Track failures, too: For Dr. Hunter’s team, some of their best data comes from tracking “failure to progress” rates. These failures illustrate when a patient has been seen for a certain number of visits but is experiencing the same amount or more pain than the previous visit. If they observe the failure rate increasing, they can make swift adjustments to the care plan to improve their status.
- Aim for continuous improvement: When collecting data, clinics may start to notice mistakes in their processes that lead to failed outcomes. But noticing mistakes can be a powerful teacher. Being comfortable with that reality can lead to amazing breakthroughs in research, as long as you aim to improve continuously.
The Continuous Process Simplification Model
While process improvement is important, simplifying the process as much as possible for the therapist should also be prioritized. As a final piece of advice, Jerry Henderson, PT, shared his Continuous Process Simplification model to refine clinic processes. Here’s how it works:
- Eliminate friction: Aim to automate compliance processes, use simplified templates and a user-friendly system, and work at removing barriers to care for therapists, so patients receive the best care during their visit.
- Push information: Instead of pulling the patient through the care process model (CPM), aim to push the information they need when they need it. With automated systems, providers can easily send patients a pre-designed home exercise program (HEP) or other educational materials to help the patient stay engaged and compliant with their care plan.
- Measure results: Ask for and track patient-report outcomes (PRO) to understand your care plan’s effectiveness. Also, consider measuring results for clinic financials, patient voice and feedback, and functional measurements to refine those processes further.
- Improve processes: Take all the information learned along the way, adjust the processes as needed, and apply relevant learnings to the next patient visit.



Comments