John Woolf, PT, ATC, COMT is the founder and CEO of Patient Success Systems, a training and consulting company that guides organizations to better evidence-based patient engagement. He can be reached at jwoolf@patientsuccesssystems.com.
Patient satisfaction is one of many patient-reported outcomes that organizations use to measure clinical success. In fact, patient experience has been identified as an important aim in healthcare and a crucial value-based measure for reimbursement.
That said, achieving patient satisfaction is about more than simply getting a good NPS score or Google review. There is a strong argument that clinical outcomes are directly related to patient satisfaction—an argument that appears to be supported by research. Let’s take a closer look as to why.
Patient satisfaction correlates with completion of care
The degree to which a patient is satisfied with their experience is likely going to influence whether they complete a plan of care. That’s because we know that if patients complete a plan of care, they are more likely to realize the benefits of therapy. But if they don’t stick with the plan, they may not.
It is widely agreed that patient satisfaction is a challenging variable to study. However, a 2020 systematic review by Rossettini and colleagues provides some helpful insights about the determinants of patient satisfaction. They conclude that patient satisfaction:
- “Is a self-reported outcome that is complex, dynamic, implicit, subjective and a multidimensional construct.”
- “It involves cognitive, affective and emotional processes through which the patient evaluates the congruence between the overall actual healthcare experience and her needs, values, desires, and expectations.”
- “The higher the congruence between the actual experience and the patient’s expectation, the greater reported level of satisfaction.”
Satisfaction is an emotional process. It involves cognitive and analytical functions, but it also involves emotional centers in the patient’s brain.
Perceived value varies between individuals
Think of the last time you went to a restaurant and left unsatisfied with the experience. Can you remember the ways in which you were not satisfied? Did you go back? Why or why not?
Have you ever had an experience where the food was excellent, but the service was poor? Or vice versa—where the service was great, but the food was lousy? Which of these is more important to you? If you had to choose between having great service with mediocre food or great food with terrible service, which would you prefer?
As for me, I like good food, but if the service is not up to par, my total experience is diminished. My wife is different; she used to be a waitress in college, so she’s much more patient with the servers when we go out to eat. This illustrates that people have different sorting criteria as to what makes for a “valuable experience.”
There are many variables you may consider before deciding that something is satisfying. Satisfaction with an experience will influence the likelihood of returning to that place.
Allow me to provide a simple working model:
At multiple points during their care, the patient must decide if it’s “worth it.” This means determining if the time, energy, cost, and effort are valuable enough to proceed. But how does a patient decide if the care is genuinely worth it? Consider a scale that can be tipped in either direction. In the process of deciding, the simple and safe assumption is that the perceived value must outweigh the perceived costs.
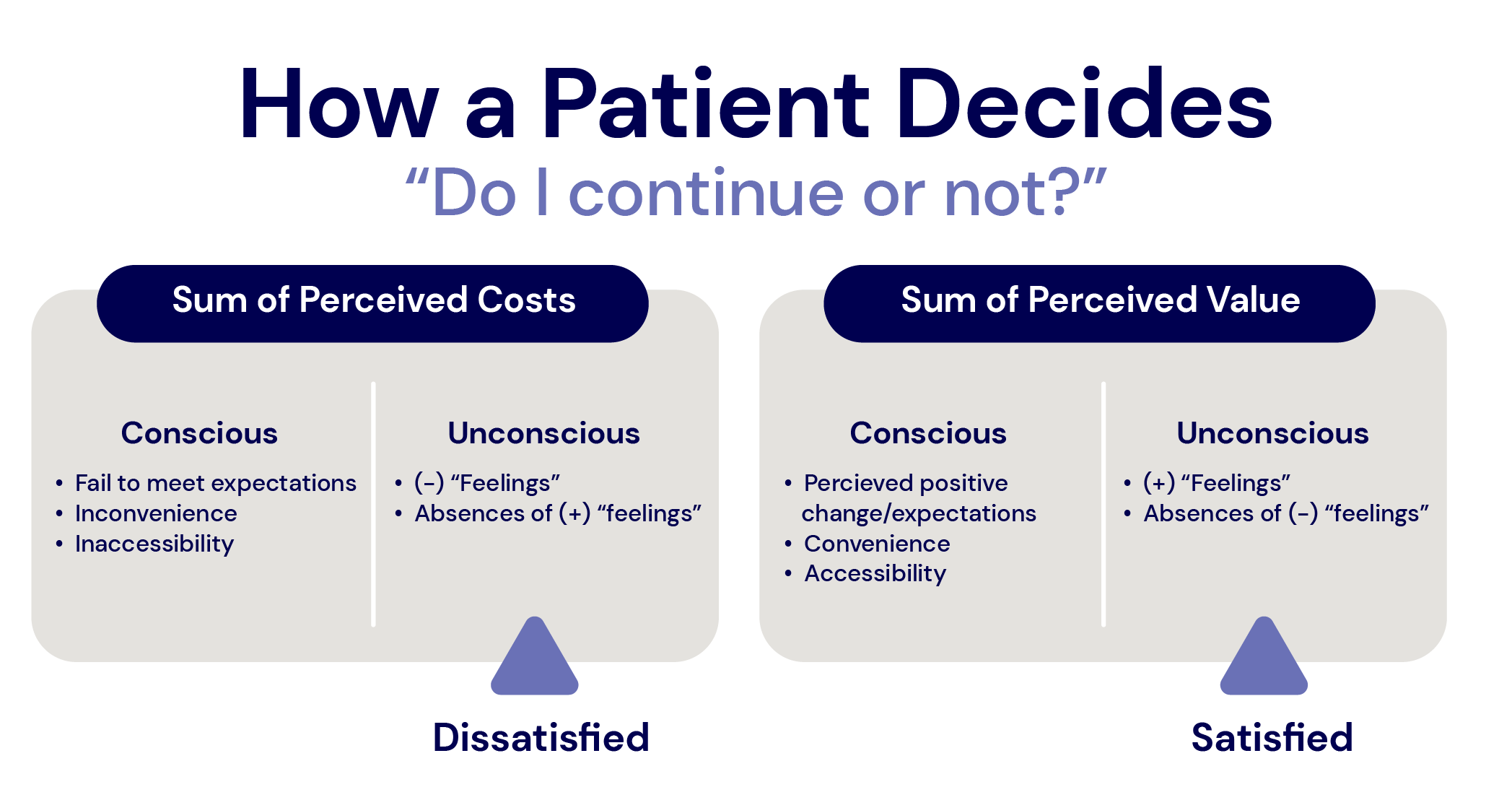
The key term in the equation is perception—the sum of conscious and unconscious experiences. The patient’s perception of the value and costs will determine the direction in which the scale tips.
Conscious variables include financial factors, their own expectations, convenience aspects such as accessibility, scheduling, or difficulty with the system required to get care. However, what may not be readily known to the patient are unconscious feelings. The part of the brain that is assessing all variables in the encounter to determine if it “feels good.”
For example, think of a time where you entered a place, and it felt “good.” Recall the energy of the environment that you picked up on or its overall vibe.
Within that subconscious set of emotions may be a sense of belonging, safety, and other feelings that humans use to decide whether something is “right” for them. To make these assessments, we use systems associated with the amygdala—the part of our brain responsible for generating emotions that move us in one direction or another. I can confidently say that some patients are willing to pay more and travel further to feel that they are well cared for and belong. These patients “feel” a heightened sense of satisfaction, and thus, the perceived value keeps them engaged and coming back.
Three themes in patient satisfaction
Research can help us understand these concepts. Another systemic review by Hush and colleagues in 2011 identified three themes within patient satisfaction: the organization of care, the process of care, and the therapist’s attributes.
- Well-organized care – The degree to which care is well-organized matters. This may include aspects such as:
- Ease of access (parking, location) and reasonable hours
- Convenient appointment options (like online scheduling)
- A helpful administrative staff
- Low wait times in the lobby
- Bill responsibility communicated clearly and easy to pay
- And giving the premise of functioning under high standards of care
- Process of care – These factors may sound familiar:
- The perception that the duration and frequency of care were adequate
- The perception that follow-up processes were appropriate
- The continuity of care and mode of treatment
- The degree to which the patient participated in the decision-making
- Therapist’s attributes – The most consistent determination in all reviewed studies was the therapist’s attributes. These include the patient’s perception of the therapist’s:
- Skill
- Knowledge
- Professionalism
- Friendliness
- Ability to effectively communicate—specifically, “an ability to provide a helpful explanation about the patient’s condition and prognosis and the ability to clarify the patient’s role in the treatment process.”
Interpersonal aspects are vital in patient satisfaction
The authors concluded: “The professional’s interpersonal aspects have been identified as the most important determinants of not only patient satisfaction but also the patient’s evaluation of the quality of care.” For instance, attributes of empathy and interaction that allowed patients to feel they are not only being heard but also treated with sympathy and respect.
If you think about it, patients rarely know, within their cognitive perception, if they are getting a properly executed lower back or shoulder mobilization or whether the ultrasound was performed with the correct settings. However, patients can and will sense the therapist’s skill by the degree to which they can communicate what they know in a manner that is both professional and, at the same time, approachable and friendly.
The patient “feels satisfied” when the therapist connects with the emotions of the patient’s experience and creates clarity by explaining what the problem is and how it can improve.
One somewhat unexpected finding from the Hush (et. al) study? Patient satisfaction with physical therapy care is determined more by interactions with the therapist and the process of care than by the actual treatment outcome.
In my personal experience, I have had multiple occasions when I could not help my patient with what they needed and had to refer them to another referral source or colleague. However, the patient would tell me how much they appreciated my efforts and would be back if another need arose. They were satisfied with the experience even though they did not reach a satisfactory clinical outcome.
This is an example of a completed plan of care wherein the completion of the care is not because the patient met their clinical goals. Instead, a mutual agreement was made that a change to their plan of care would bring my treatment of the condition to an end.
But suppose a patient does not perceive their experience with you as valuable. In that case, there is an increased likelihood that your patient will not complete a plan of care and will label the experience as a “failed intervention.” And it may not even be because of your technical skills, but rather the patient’s perception that the experience was not valuable.
That’s because you can be the best technically-trained therapist and still fail to connect with the patient.
Final thoughts
We want our patients to stay engaged with the treatment plan. We know that if they stay engaged, they will gain the benefits of the treatment. Their bodies and minds will adapt, and they will achieve their goals.
Still, it’s important to remember that therapy is a process. It is a journey that takes time and energy. For most, there is a perceived cost and a perceived benefit. The result will be the overall perceived value.
We need to continue our journey to becoming more psychologically informed. Research that explores patient satisfaction is valuable, and research shows the interpersonal attributes of the provider is important for satisfaction. With this framework, we can dive deeper into the underpinnings of the patient experience to better understand how these attributes contribute to relationship-centered care and better outcomes.
—
Looking to increase patient satisfaction, but unsure of where to start? We have a few ideas, including improved access to your clinic schedule and virtual appointment options. Request a free demo of Insight and BetterHealthcare today to learn more.
—
Sources:
1Rossettini, G., Latini, T. M., Palese, A., Jack, S. M., Ristori, D., Gonzatto, S., & Testa, M. (2020). “Determinants of patient satisfaction in outpatient musculoskeletal physiotherapy: a systematic, qualitative meta-summary, and meta-synthesis.” Disability and Rehabilitation, 42(4), 460-472. View Article Here
2Hush, J. M., Cameron, K., & Mackey, M. (2011). “Patient Satisfaction With Musculoskeletal Physical Therapy Care: A Systematic Review.” Physical Therapy, 91(1), 25–36. View Article Here




Comments