Editor’s Note: This article is a guest contribution from Patient Success Systems co-founder, John Woolf (MS, PT, ATC, COMT).
As the former owner of a successful practice, I recall continually striving to provide the best possible experience for our patients. This ongoing process entailed a review of best practices, internal reflection, and an examination of every aspect of the patient experience, including the website, phone interaction, the parking, and the clinic space. I knew that as the patient’s out-of-pocket costs increased, we had to make continual efforts to increase the patient’s perceived value of our care. We learned that patients were more likely to pay for the necessary visits to complete a plan of care if they perceived a high level of value.
I also understood that our growth was dependent upon a steady stream of “high-value” experience. Patients were referred to us from multiple professional sources, such as referring physicians. However, we slowly noticed how consolidation influenced the flow of referrals to their “in-house” therapy. This was a significant threat to the health and growth of our company that invited a deeper dive into our core values and the operational integrity around those values.
We brainstormed ways to ensure that our facilities were appealing and accessible, provided easy scheduling access, and allotted adequate time for patient visits. It was through this focused introspection that led us to the conclusion that our mission was to be a Relationship-Centered healthcare company. Yes, we were physical therapists providing excellent technical skills, but in order to fully thrive, we had to focus on the relationship with our patients.
What does empathy have to do with it?
It was only after my transition from the “school of private practice” to a Ph.D. program in performance psychology that I finally gathered language to better describe what we knew then—and I believe it still applies. Yes, patients want high value, but what is it that patients value most?
There has been a recent surge in published research investigating this question (for a complete list, contact me at jwoolf@patientsuccesssystems.com). Hush et al. (2011) conducted a systematic review of the literature published on the topic of patient satisfaction and found that the “the most consistent determinant of patient satisfaction across all studies[…]was the therapist’s interpersonal attributes, (p.33, emphasis added)1” specifically, knowledge, skill-friendly attitude, and effective communication. An unexpected finding was that the actual treatment outcome, although important, was not a consistent determinant of satisfaction with physical therapy care.
In a more recent study, Rosettini et al. (2020) essentially repeated the systematic review of the literature and illustrated the important association between all the factors that contribute to patient satisfaction. They concluded that patient satisfaction is a confluence of multiple variables, including not only clinical outcomes but also contextual factors such as the physical therapist’s “features” and the therapist-patient relationship.2
But wait! How could the treatment result not be the most important determinant of a satisfied patient? Is it possible that patients value more than the treatment outcome? My professional experience, and some scientific evidence, would suggest yes.
Patients obviously want a clinical outcome. However, they have to engage in a process that “feels good” to achieve that outcome; they have to stick to the treatment plan. If they don’t stick to the treatment plan, they may fail to get the necessary (physical and learning) adaptation to realize the outcome. They have to stay engaged in the process, but many patients will continually ask, “Why would I go to see my PT twice a week, take time from a busy schedule, and likely pay a high co-pay?”
Because it “feels” good.
Not just in the sense of relief from pain but also from the connection with the therapist and the rest of their team helping the patient heal. The patient wants to go to PT because they feel like the team is there for them, genuinely cares about their progress, and views the patient as an important part of their lives.
Finally, empathy!
What does empathy mean today?
Empathy is commonly used as a condition for successful clinical engagement. German philosophers initially used it to understand how a person could “feel into” or have an emotional experience with an inanimate object, such as a work of art or nature. It is a process of “stepping into the other.”
Empathy retains a similar meaning these days but is now more commonly used to describe how we connect with another person’s experiences. From an evolutionary and social perspective, empathy is a vital function that keeps us connected. Under the best circumstances, we use empathy to assist one another through difficulties.
Empathy is the culmination of three psychological processes:
- Mindreading, whereby our brains engage in a process of understanding another person by mentalizing or deciphering the context of their situation. This is a mind function that we all do all the time. We see another person’s actions or expression, and our minds try to make sense of it by inferring meeting. We may also engage our brain’s mirror system to replicate the image of their situation in our minds and gauge the other person’s intent.
- Affect matching, where we utilize the part of our brain and the mechanisms supporting social pains that allow us to actually feel the other person’s experience.
- Empathic motivation, whereby we engage the brain’s septal region that motivates us to act, do something, and engage.
It is not true empathy unless we can link all three components effectively.
Empathy within a clinical environment
In a healthcare environment, empathy is not something that we “do” to another person, but rather a process where we engage with our patient on an emotional level, often unconsciously. It supports the innate social networks of our brain and provides both the patient and provider a sense of “belonging, safety, and trust.”
When this process is successfully activated, we engage in the process of Interpersonal Emotional Regulation (IER), wherein both the patient and provider join in influencing the emotional state of the other in a positive direction. The empathy process creates the holistic feeling of “I am seen, I am important, I am connected, and I am safe.” It creates an optimal emotional state for the patient and provider to succeed.
Our patients are stressed. The injury or affliction has negatively impacted their lives. They are often anxious, angry, fearful, and, at worst, hopeless. The pain science literature informs us that our chronic pain folks are on a constant overdrive of the HPA axis—meaning they are in a continual state of emotional dysregulation, where the negative chemistry is continually flowing. These emotional states are not ideal for creating a healing response. We can help by engaging in the process of empathy.
A successful process of empathy will help the patient quell the anxiety often associated with a healthcare visit. The provider’s skill at regulating their own emotions and communicating (verbally and non-verbally) in a manner that includes affect matching, reflective stance, and a sense of “we are similar” will be a significant determinant as to whether or not the patient feels good about the encounter.
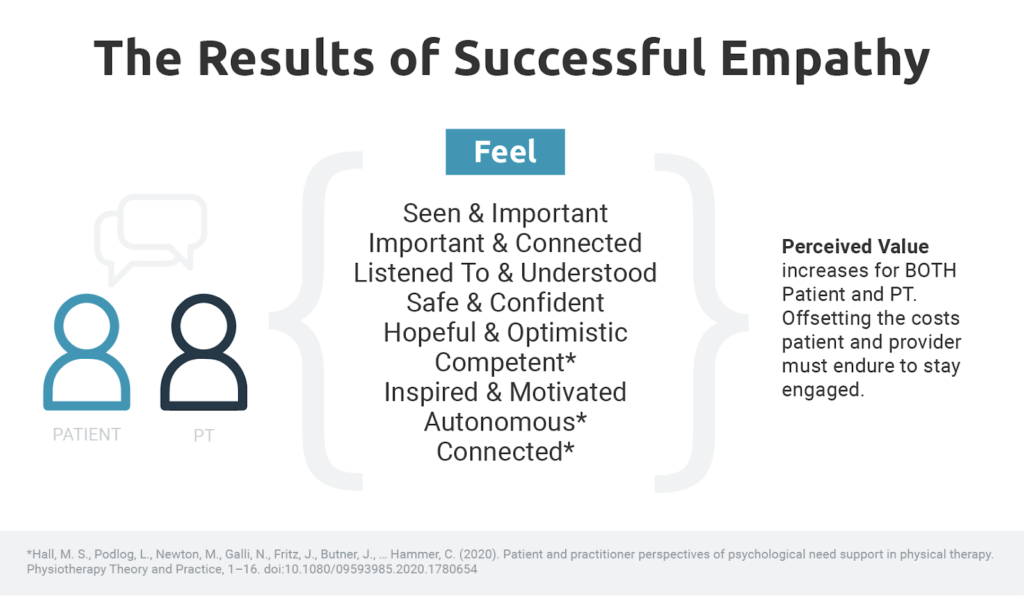
When a patient “feels good” when working with us, because we establish an empathetic connection, they are more likely to place a higher value on the process. In doing so, their motivation to attend will increase, they are less likely to cancel or no-show, and they are more likely to complete a plan of care. Therefore, they are more likely to achieve their clinical goals because they remain engaged in the process.
In part two of this series, Three Ways Empathy Can Work Against You, we uncover how empathy, if not done properly, can have very serious consequences, including compassion fatigue and burnout. It can also increase a patient’s anxiety and minimize the odds of the patient sticking with you for the entire plan of care.
—-
References:
1Hush, J. M., Cameron, K., & Mackey, M. (2011). Patient satisfaction with musculoskeletal physical therapy care: a systematic review. Physical therapy, 91(1), 25-36.
2Rossettini, G., Latini, T. M., Palese, A., Jack, S. M., Ristori, D., Gonzatto, S., & Testa, M. (2020). Determinants of patient satisfaction in outpatient musculoskeletal physiotherapy: a systematic, qualitative meta-summary, and meta-synthesis. Disability and Rehabilitation, 42(4), 460-472.




Comments