By now, you have heard that PTs and OTs will be eligible to participate in the CMS Merit-based Incentive Payment System, or MIPS, beginning in 2019. We believe that MIPS represents a sea change event, it is an important milestone in the transition from fee for service to value-based care.
For Medicare providers, success in MIPS is essential. But, history has shown that commercial payers emulate programs that are developed by CMS within the Center for Medicare and Medicaid Innovation. For non-Medicare providers, understanding MIPS concepts and incentives will become increasingly important as other payers begin to embrace programs that incentivize value over volume.
Background
MIPS has been in effect for physicians and some nurse specialists since 2017. It is designed as a hybrid program for providers who are not able to participate in other Advanced Alternative Payment Models. It leaves the current fee for service system in place without annual increases in the fee schedule; combined with a complex series of financial incentives designed to improve quality and service to beneficiaries, improve the use of electronic records, and decrease costs.
The CMS Notice of Proposed Rulemaking published on July 27th indicates that physical therapists and occupational therapists will be eligible to participate in MIPS beginning on January 1, 2019. Speech language pathologists will likely not be eligible in 2019 but will likely be eligible in subsequent years (edit: we have since learned in the final rule that SLPs are included as MIPS eligible providers in 2019).
Feeling lost in a fog of MIPS terminology? Download our MIPS glossary to gain a better understanding of its common and not so common terms.
Download GlossaryConcepts
Based on data submitted by providers for a “Performance Year” plus claims data, CMS calculates a 0-100 point MIPS score. The MIPS score is used to assess a financial bonus or penalty to be applied to the fee schedule, or “Payment Year”, two years later. For example, MIPS performance in 2019 will affect the Medicare Fee Schedule, negatively or positively, in 2021.
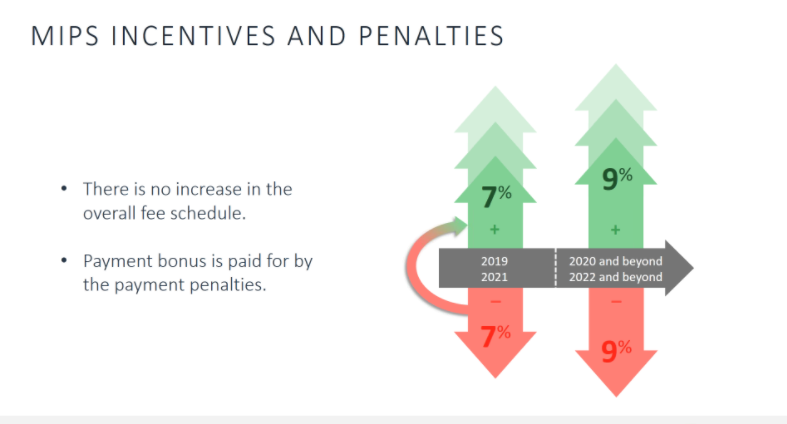
Based on your MIPS score for 2019, your Medicare payments for 2021 could increase or decrease by as much as 7%. In fact, there is an opportunity to earn a bonus that is even greater than 7% in the 2019 payment year.
Similarities to PQRS
This methodology for assessing financial incentives may sound somewhat familiar for those of you who participated in the PQRS program which ended in 2016. And, indeed, part of the MIPS program has its roots in the, now defunct, PQRS program. In fact, it turns out that for PT and OT, 85% of the MIPS score is based on the Quality Measures component and Quality Measures (as published by CMS) are simply a new version of the old PQRS measures. But, just to complicate things a bit more, there are multiple methodologies for submitting and calculating MIPS scores. We will discuss the specifics around MIPS reporting methods and the advantage and disadvantages of each in future articles.
Feeling lost in a fog of MIPS terminology? Download our free MIPS glossary to gain a better understanding of its common and not so common terms.
Download GlossaryMIPS Scoring for PT and OT
As with many CMS programs, MIPS was designed for physicians first, then adapted for other provider specialties. The scoring methodology physicians included four components, but two of those components (Promoting Interoperability and Cost) are not going to be used for PT and OT. Those components along with the proposed MIPS score weighting for 2019 for physicians and PT/OT:
| Score Component | Description | Physicians | PT and OT | |
| Promoting Interoperability | Use of certified EMRs | 25% | 0% | |
| Cost | Spending per beneficiary | 15% | 0% | |
| Improvement Activities | Activities to improve clinical practice | 15% | 15% | |
| Quality Measures | Activities designed to assure quality | 45% | 85% | |
So, obviously, success in Quality Measures is an absolute necessity for successful MIPS participation for PT and OT. And, as discussed earlier, any increases in Medicare payment in future years will depend on success in MIPS.
There is More (Of Course)
The above is a very brief summary of a very complex program, and, per usual, the devil is in the details which we will discuss in future articles. Understanding these concepts is very important and will inform your decisions as you learn more about MIPS. You may decide not to participate in MIPS at all, or that going all out to participate and score highly in MIPS is a strategic goal for your practice.
It is Not Going Away
Adam Boehler, the director of the Center for Medicare and Medicaid Improvement, has made it clear that value-based systems like MIPS are not going away anytime soon and, in fact, he has gone on the record in favor of ultimately abolishing fee for service[i]. It seems obvious that the pace of the transition from fee for service to value is accelerating and that MIPS is the next incremental step toward a completely value-based system, so developing competencies around reporting MIPS Quality Measures and Improvement Activities will serve you very well in the near future.
Coming: Financial Implications, Scoring Details, Preparing for MIPS
Lack of preparation for MIPS will mark the end of life for some practices and a great opportunity for others.
As we continue this series, we will provide additional information you need to understand MIPS. We will lay out the practical considerations of MIPS participation, secrets to success with MIPS, and how a good MIPS implementation will pay more dividends than just improved Medicare payment. We will include pro-forma financial examples to demonstrate just how important MIPS may be to the financial future of your practice.
Disclaimer: The information provided herein is intended to be general in nature. It is not offered as legal or insurance related advice, and is not a complete description, or meant, or intended, to replace or be interpreted as specific, of Medicare requirements. Although every effort has been made to ensure the content herein is correct, we assume no responsibility for its accuracy. Contact Department of Health & Human Services (DHHS) Centers for Medicare and Medicaid (CMS) Services for more information.

Comments