According to CMS, 600,000 clinicians will participate in MIPS under the Quality Payment Program. Even so, confusion remains around participation options and when discussing the MIPS program with peers, I’m still surprised by how many false theories are floating around. It’s no wonder our community of physical and occupational therapists are confused.
First, let’s get some acronyms down:
- MACRA – The Medicare Access and CHIP Reauthorization Act: MACRA was introduced in 2015 with the ultimate goal of population-based payment, or capitation, and by law requires CMS to implement an incentive program to move physicians to value-based care. This incentive program is referred to as QPP.
- QPP – Quality Payment Program: QPP provides two programs, or participation tracks, which are:
- MIPS – Merit-based Incentive Payment System: MIPS eligible clinicians will be subject to a performance-based payment adjustment through MIPS.
- AAPMs – Advanced Alternative Payment Models: Take part in an AAPM? You may earn a Medicare incentive payment for sufficiently participating in a new payment model.
Next, let’s set the record straight and debunk these five following MIPS myths.
1. MIPS is just another Medicare program
False! MIPS is NOT just another Medicare program. The MACRA legislation passed with bi-partisan support by Congress in 2015 mandated the transition of our healthcare reimbursement system from fee-for-service to fee-for-value, by declaring an ultimate goal of transitioning to capitated payments.
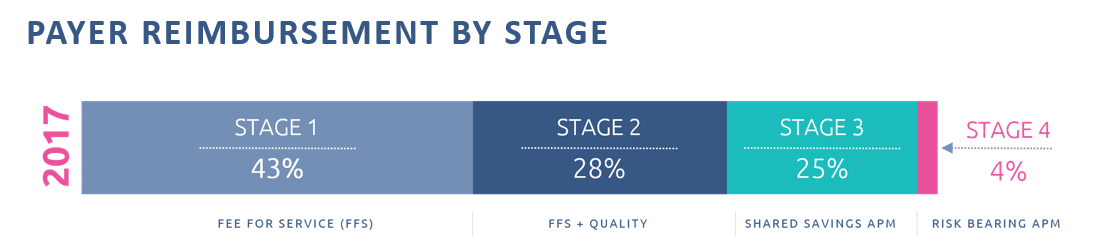
The Quality Payment Program created through MACRA defines three distinct stages for the transition to fee-for-value and the MIPS component represents the foundational first step of that transition. The QPP was designed to give providers the time they need to develop the operational competencies needed to successfully participate in these new payment models. If you delay participation in MIPS, you are effectively robbing yourself of the time and assistance you need to successfully transition to value-based care.
The cost of healthcare in the United States continues to skyrocket and Congress understands that true reform cannot be implemented in a fee-for-service reimbursement system.
2. MACRA, which created the Quality Payment Program and MIPS, will eventually be repealed.
Contrary to popular belief, MACRA was passed with overwhelming bipartisan support and no one in Washington has proposed repealing the legislation, despite our current hyper-partisan environment. Broad Congressional support of the legislation is based on the stark reality that Medicare is currently projected to become insolvent in 2026 and drastic interventions are required to save the program.
In addition, rapidly accelerating health care costs continue to constitute a credible threat to our economy. Healthcare is projected to consume nearly 20% of our total economy by 2025 which is widely accepted to be unsustainable. Repealing MACRA now would result in the acceleration of Medicare’s insolvency and a very negative impact on the overall economy, neither of which are viable options in our current environment.
3. I failed in PQRS so MIPS will be the same.
While MIPS has similar qualities to PQRS, it has an entirely different path and consequence for not participating. Quality reporting is just one portion of MIPS. If you are a provider thinking you’ve ‘escaped’ quality reporting because PQRS is no longer around and you aren’t required to participate in MIPS, you aren’t seeing the entire picture. Unless you don’t treat Medicare patients, are okay with accepting a frozen Medicare reimbursement rate, and/or aren’t concerned with getting behind in the value-based care transition, it’s important to understand the effects of not participating in the program.
Feeling lost in a fog of MIPS terminology? Download our MIPS glossary to gain a better understanding of its common and not so common terms.
Download Glossary4. It doesn’t make sense for Physical Therapists to voluntarily participate.
By not participating in MIPS, you forgo any possible financial benefits. While MIPS is staying optional for roughly 90% of therapists at the moment, many providers do not understand that MACRA essentially froze Medicare reimbursement starting in 2020, with only minimal increases of <1% moving forward (+.25% through 2019 and then another .25% in 2026 and beyond). So, what do you do if you want and/or need to continue receiving a pay raise from Medicare? Participate in MIPS or Alternative Payment Models.

5. MIPS is the end game
Wrong again, MIPS is NOT the end game. Through the creation of the Quality Payment Program, Medicare has provided a glide path for the transition to fee-for-value and the first step of that journey is MIPS, which ties quality performance to reimbursement. Moving further down the timeline, CMS is ultimately looking towards capitation which is expected in 7-10 years. By not participating in MIPS now, you are only setting yourself up for failure in the transition from fee-for-service to value-based care.
Disclaimer: The information provided herein is intended to be general in nature. It is not offered as legal or insurance related advice, and is not a complete description, or meant, or intended, to replace or be interpreted as specific, of Medicare requirements. Although every effort has been made to ensure the content herein is correct, we assume no responsibility for its accuracy. Contact Department of Health & Human Services (DHHS) Centers for Medicare and Medicaid (CMS) Services for more information.

Comments