Review
In prior articles, we discussed MIPS Basics and some of the practical implications of MIPS reporting. We included information on MIPS eligibility and reporting methods.
In this article, we will take a closer look at MIPS scoring and financial incentives.
Score Components
Physicians and some nurse specialists have been eligible to participate in MIPS since 2017. For those specialties, MIPS scoring for 2019 is based on four weighted categories: Promoting Interoperability, Cost, Quality Measures, and Improvement Activities.
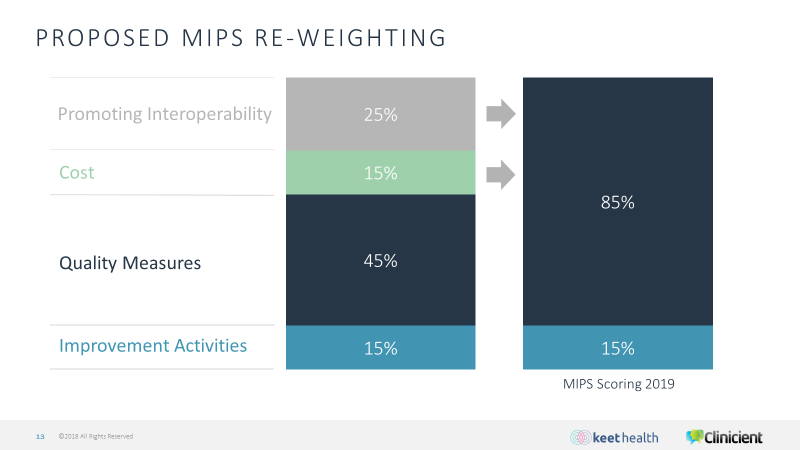
The Promoting Interoperability and Cost components will not be part of MIPS scoring for PTs and OTs, and the weighting of those components are being transferred to the Quality Measures component, as shown on this graphic.
MIPS Quality Measures
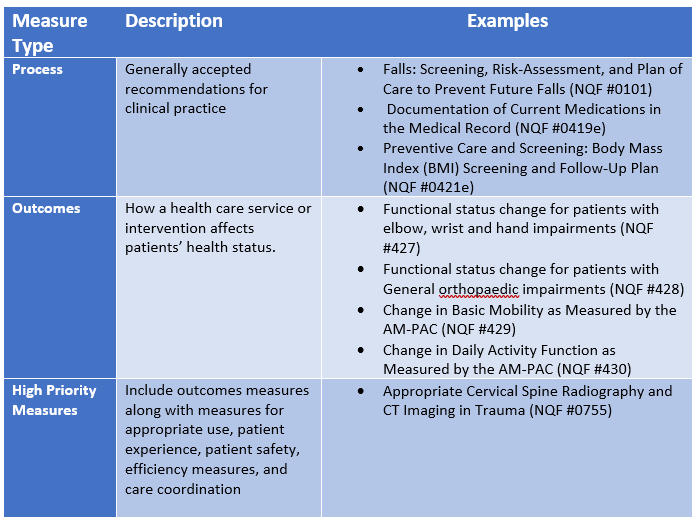
Based on the above, it is obvious that scoring well with Quality Measures is critical to success for PTs and OTs. Unlike the old PQRS program, Quality Measures have variable values. Quality Measure types that are approved by the National Quality Forum (NQF) are utilized in claims and traditional registry reporting. The measure types are illustrated below:
Success in Quality Measures
As stated earlier, Quality Measures count for 85% of the total MIPS score for PT and OT. Based on the latest information from CMS, you must submit a minimum data set of six Quality Measures for a minimum 90 day period, but will need to report over a longer period to obtain a higher score and increase your chances of attaining a positive payment adjustment.
Process measures are valued at 3 points each. Higher valued outcomes measures are worth from 3 to 10 points if the measure can be scored against historic benchmarks.
With the exception of outcomes measures, many of the other high value measures are not applicable for PT and OT. So, the key to succeeding in MIPS Quality Measures for PT and OT are to report on outcomes measures over the course of the entire year that may be compared against historic benchmarks.
Feeling lost in a fog of MIPS terminology? Download our MIPS glossary to gain a better understanding of its common and not so common terms.
Download GlossarySuccess with Improvement Activities
Improvement Activities are primarily reported via an attestation process and count for the remaining 15% of the composite MIPS score. Similar to Quality Measures, not all Improvement Activities are created equal. High scoring for Improvement Activities requires reporting on 2 high-weighted activities, 1 high and 2 medium weighted activities, or 4 medium-weighted activities.
Currently, there are 113 published improvement activities, and approximately 30 of them are applicable for PT and OT. Among the high weighted activities:
- Collection and follow-up on patient experience and satisfaction data on beneficiary engagement
- Promote Use of Patient-Reported Outcome Tools
Some examples of medium weighted activities:
- Collection and use of patient experience and satisfaction data on access
- Improved Practices that Engage Patients Pre-Visit
- Leveraging a QCDR for use of standard questionnaires.
Closer Look at Financial Incentives
To review, success in reporting MIPS Quality Measures is of critical importance for PT and OT, and there are significant financial implications for those who are required to participate, or choose to opt-in.
At a minimum, there is a potential 7% bonus for successful MIPS participation which is totally paid by a pool of providers who receive a financial penalty for unsuccessful MIPS participation of up to 7%. But, in addition to the potential 7% bonus, there are 2 pathways to exceed a 7% bonus in the 2019 performance year:
- If the total amount of provider penalties exceeds the total amount of provider bonuses, providers in the bonus pool could (theoretically) receive up to a 3x increase in the bonus. (It should be noted that the likelihood of having an excess in the penalty pool to distribute to the bonus pool is low.)
- There is also an entirely separate bonus pool of $500M, which is distributed to the providers in the highest quartile of performers, up to 10% for providers in the 99th So, there is a realistic opportunity for a 17% payment bonus in payment year 2019.
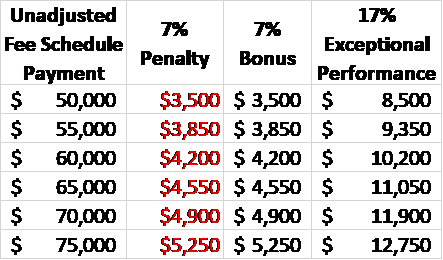
You may estimate your financial risk or potential bonus payments by using your 2018 Medicare payment data and creating a simple spreadsheet. Here are some examples for therapists with between $50,000 and $75,000 in allowed Medicare payments for performance year 2019.
Coming: Preparing for MIPS
In our next article in this series, we will provide a series of concrete steps you should begin taking now to prepare for MIPS.

Comments