It’s that time of year again: PQRS update time. Toward the end of every year, CMS informs therapists if they failed to participate in PQRS correctly the previous year.
Before we discuss what is on the PQRS horizon, and what to do if CMS sent you a letter about your PQRS performance, let’s review the basics of the reporting program.
PQRS Refresher
The Physician Quality Reporting System (PQRS) is a voluntary Medicare quality reporting program. The system is designed to provide incentives for providers to report that they completed certain tasks designed to improve quality.
Below are three things you must understand about the program:
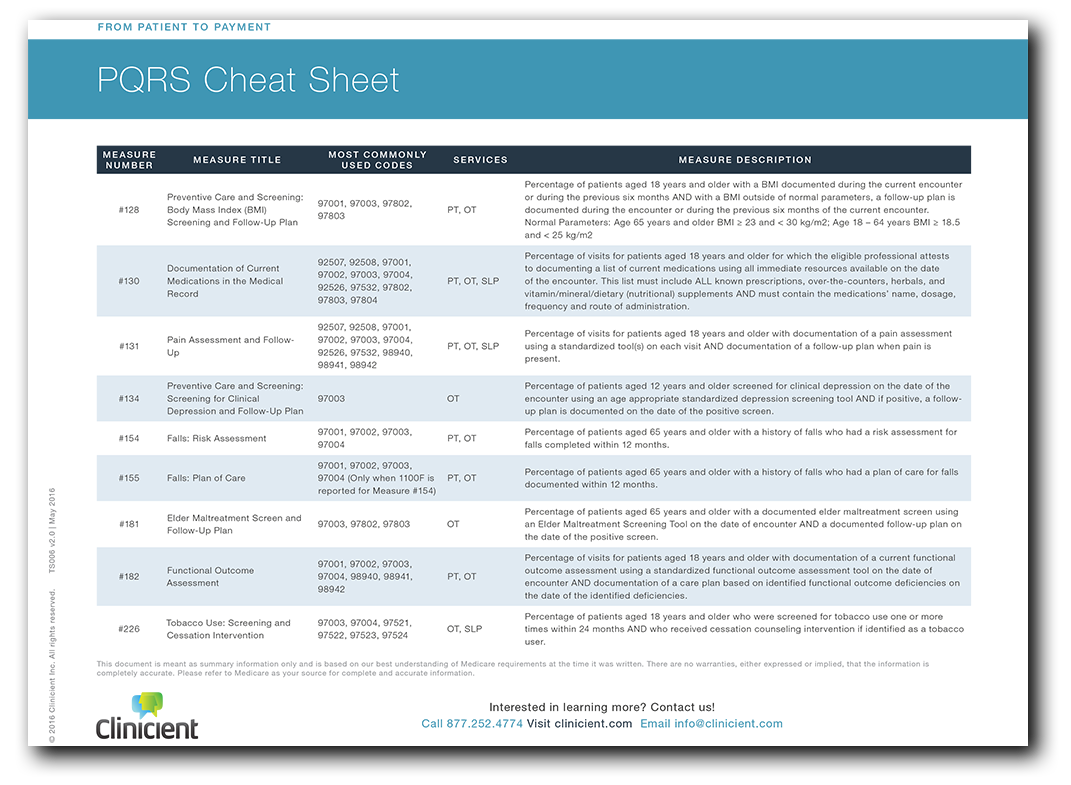
- Acceptable PQRS Measures for a Visit are Based on Various Factors- These factors always include the patient’s age and other procedures performed during the visit. Some measures require additional factors for eligibility, like the patient’s diagnosis, or the results of other related PQRS measures.
- You Must Report on All PQRS Measures, 50% of the Time- As of January 1, 2015, the successful reporting requirements for physical therapists, occupational therapists and speech therapists were increased to require reporting on all measures on at least 50% of the eligible visits.
- Your Current PQRS Performance Impacts Payments in Two Years- Originally, the program offered a small financial bonus for participation. More recently, the bonus incentives were phased out and replaced by financial penalties for non-participation.
The penalties for non-participation are levied two years after CMS analyzes PQRS data. So, as determined by Medicare’s minimum participation requirements, a 2% penalty in 2017 payments would be levied for non-participation in 2015, and a 2% penalty in 2018 payments may be levied for non-participation in 2016.
Clinicient PQRS Support
In the INSIGHT platform, the appropriate list of eligible PQRS measures will pop up automatically at sign off, based on the patient’s age and other procedures performed during the visit (eval, re-eval, manual therapy, etc), and, for some measures, the patient’s diagnosis and other factors. All that you need to do is check off the applicable measures that were completed, and the appropriate PQRS “G Codes” will be included on the claim automatically.
Common PQRS Mistakes
Despite the automation of PQRS reporting in the Clinicient system, clients have stumbled in two common ways that technology cannot prevent: “Performance not Met” and “Fall Risks Plan of Care” reporting.
- “Performance Not Met” Reporting. For all of the PQRS measures, there is an option to report that the performance criteria for the measure was met, or it was not met because of a reasonable exclusion criteria, or was not met and there is no appropriate exclusion for the non-performance. Please be aware that reporting that the measurement was not performed without an acceptable exclusion does not count toward PQRS participation.
- Fall Risk and Falls Plan of Care Measures. The Falls Risk Measure (154) is “paired” with the Falls Plan of Care Measure (155) and is an applicable measure for some OT and PT patients. If you reported that the patient was not a Fall Risk in Measure 154, that patient is not eligible for the Falls Plan of Care Measure. If you do report that the patient is a Fall Risk in Measure 154, that patient is eligible for reporting on for the Falls Plan of Care. If you do not report on measure 155 when there is no fall risk on Measure 154, it does not count against your participation rate.
Did You Get a PQRS Letter from CMS?
You may have received a letter from CMS indicating that your Medicare payments for 2017 are being reduced by 2% because you did not satisfactorily report on PQRS in 2015. If you did, there are two steps you must take to prevent future payment penalties.
- Request an Informal Review– Request an informal review on the CMS Quality Net This report will indicate whether or not the measures were satisfactorily reported, and why any measures were not satisfactorily reported.
- Monitor Your PQRS Participation Rates- It is critically important to monitor your PQRS performance metrics. To monitor your PQRS participation rates in INSIGHT, select the PQRS Completion Rate report for the current year. All of your therapists should participate well above the 50% threshold.
- Train Your Staff. It is critically important that all therapists have an understanding of PQRS concepts. For example, simply reporting PQRS codes that indicate a measure was not performed does not count toward your overall PQRS participation.
What’s Next with PQRS?
CMS has not yet released its 2017 PQRS reporting requirements. As soon as the requirements are released, Clinicient will analyze them and adapt our system to support them.
There is more change to come. We will continue to analyze these complex requirements and adapt our systems to make compliance as easy as possible. We will also continue to explain how to successfully navigate PQRS along with all of the other Medicare requirements. We will produce more educational programs in the form of webinars, summary documents, blog posts, and lectures to keep you on top of these important changes.
Medicare has a number of initiatives designed to improve quality and decrease costs planned for the near future. Successful participation in current and future Medicare programs will require that providers have a good understanding of the program concepts. We will continue to strive with you to assure success as we face these challenges together.

Comments